Scleral lenses and ocular surface disease
Scleral lenses provide patients with many benefits and are an extremely useful adjunct in treating patients with ocular surface disease (OSD). Step three of the TFOS DEWS II report1 notes gas permeable scleral contact lenses (CLs) can be very beneficial to patients with moderate-to-severe dry eye disease, including Sjögren syndrome, Stevens-Johnson syndrome, rosacea, chemical burns, thermal burns, mucous membrane pemphigoid and meibomian gland dysfunction blepharitis.
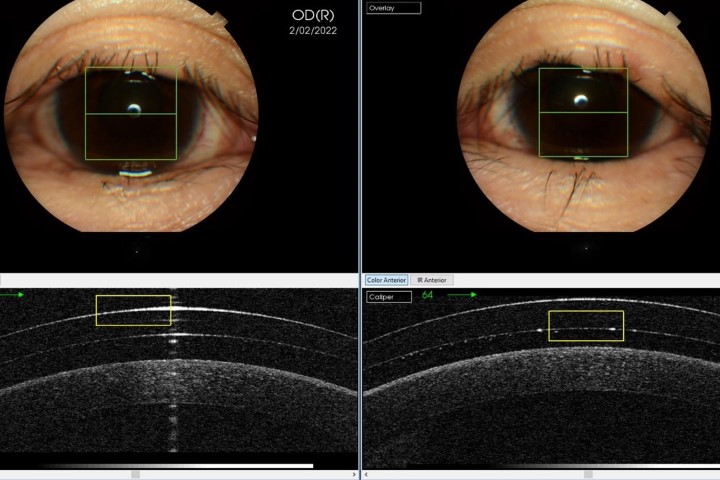
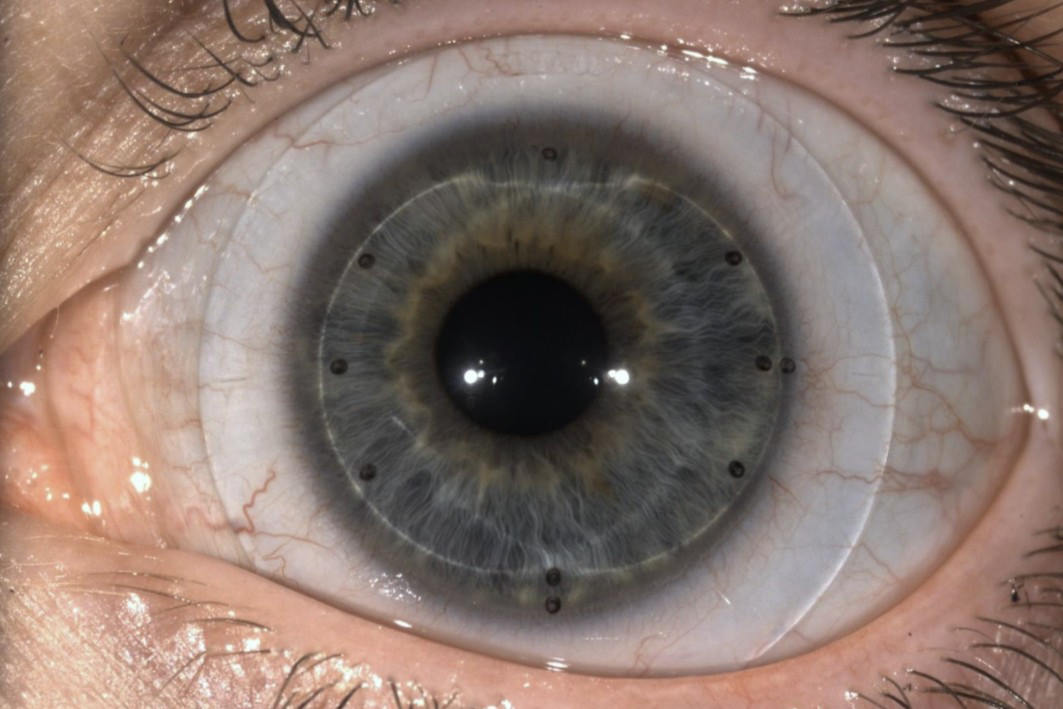
Compared to other types of CL, scleral lenses have several advantages. Firstly, by vaulting the cornea and not sitting on its surface (Fig 1, top) they minimise irritation. That space between the corneal surface and the scleral lens is filled with non-preserved saline, which acts as a constant source of hydration, which can provide significant relief for patients with dry eye disease. Secondly, since OSD can leave the eyes more sensitive and the corneas more vulnerable, blinking can irritate the eye or even cause injury due to mechanical friction of the eyelids on the cornea. Scleral lenses act as a shield, protecting the eyes from further irritation or damage, which also reduces obvious signs of inflammation and gives them a healthier appearance. Patients can also continue using preservative-free eyedrops or artificial tears to lubricate the eye during scleral lens wear, although many of my patients find they can decrease the frequency of artificial tear use.
These factors can improve the quality of life of people with dry eye disease. Scleral lenses can also aid in decreasing pain and discomfort, eye redness, the need to repeatedly rub the eyes or apply eyedrops, all while providing crisp, clear vision.
Case study
KS is a 47-year-old female diagnosed with Stevens-Johnson Syndrome in December 2018.
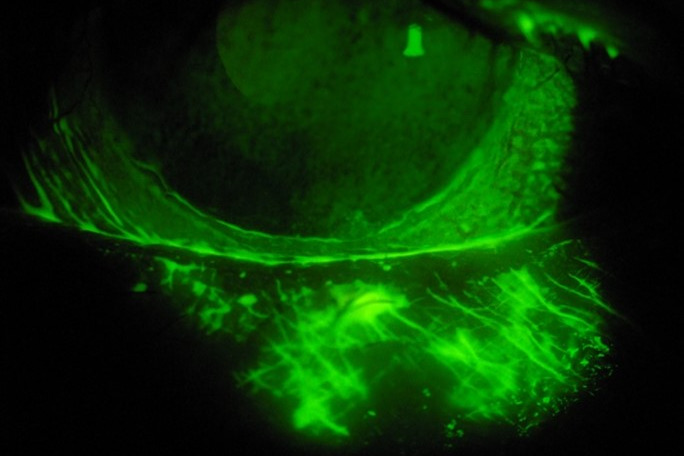
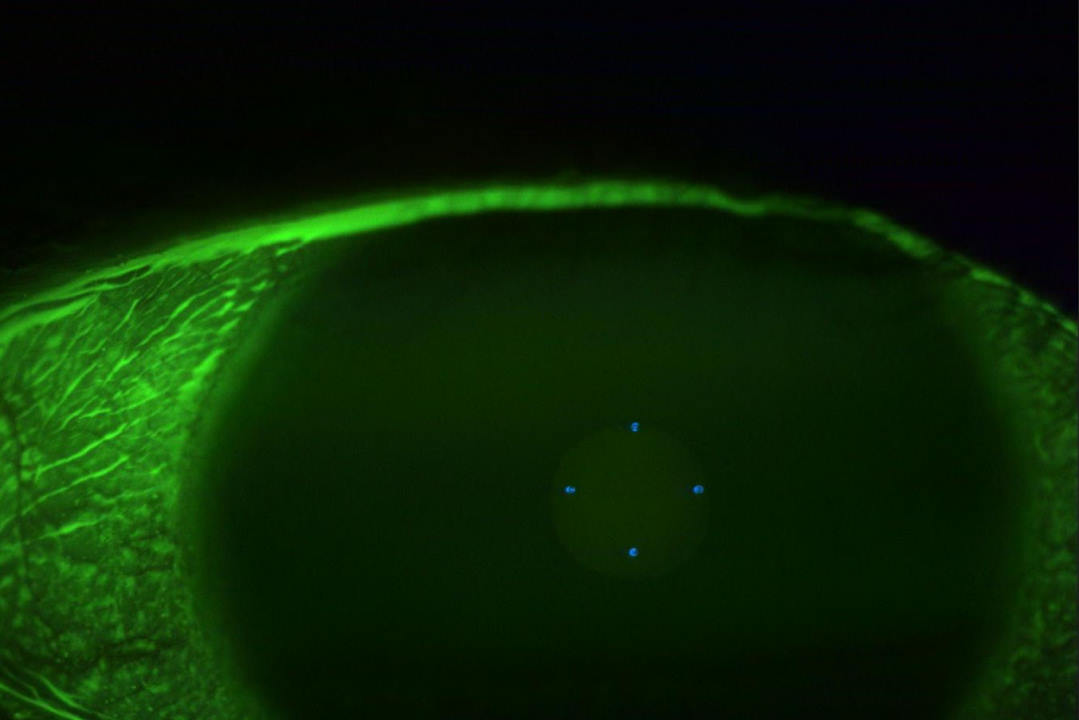
Fig 2a. Conjunctival staining at presentation
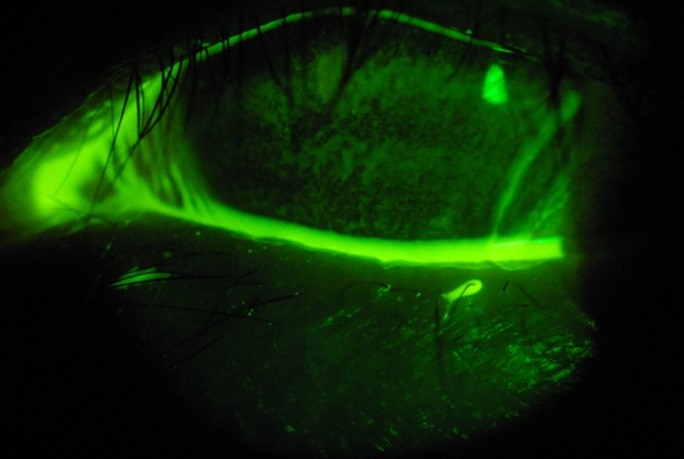
Fig 2b. Corneal staining at presentation

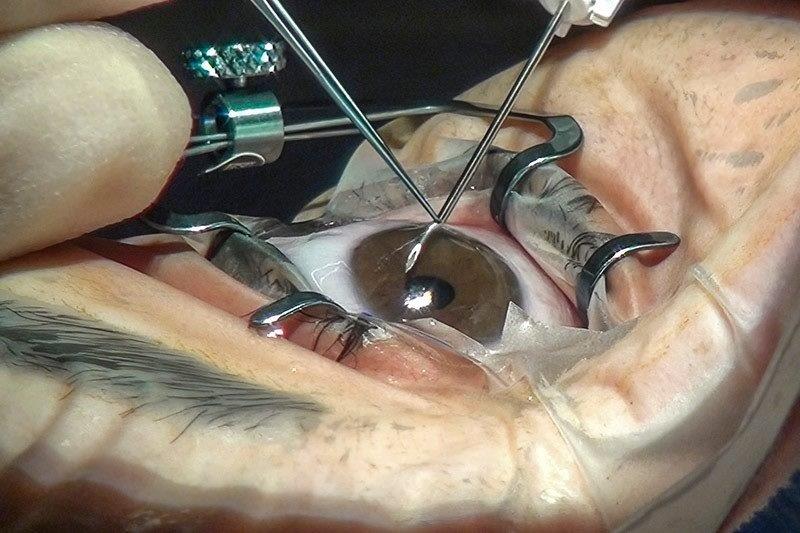
Fig 2c. KS' eye upon presentation
Typical eye problems associated with Stevens-Johnson syndrome include conjunctivitis, ulceration of the eyelids, inflammation inside the eye (iritis), corneal blisters and corneal perforation. After the acute stage of the disease, conjunctival and corneal scarring (Fig 2), which can lead to a decrease or loss of vision, are common.
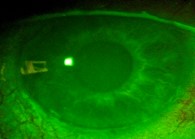
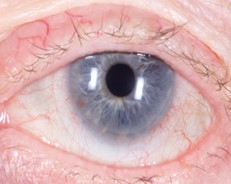
Fig 3a (left). KS' cornea with no corneal staining or desiccation. Fig 3b (right). KS' white, calm eye while wearing her scleral lens
Figs 3a and 3b show the vast improvement in the patient’s corneal integrity, along with a substantial increase in her visual acuity, after scleral lens wear. KS is achieving visual acuities of right eye 6/7.5+1, left eye 6/9.5+1 and binocular visual acuity of 6/6. She is using her serum drops from the hospital to keep the front surface of her CLs hydrated.
Reference
- Craig J, Nelson J, Azar D, Belmonte C, Bron A, Chauhan, de Paiva CS, Gomes J, Hammitt K, Jones L, Nichols J, Nichols K, Novack G, Stapleton F, Willcox M, Wolffsohn J, Sullivan D. TFOS DEWS II Report Executive Summary. Ocul Surf. 2017 Oct;15(4):802-812. Epub 2017 Aug 8. PMID: 28797892.

Damon Ezekiel owns and manages the specialist contact lens and general optometry practice, Ezekiel Eyes, in Perth, Western Australia. He is the president of the International Society of Contact Lens Specialists, co-founder of the Euro-Asian Scleral Lens Academy and, through the charity Sight for All, has taught at ophthalmology hospitals as far afield as Vietnam and Cambodia.