Save Sight Symposium 2024: ideas and innovations in eye health
The 2024 Save Sight Symposium was held at Te Wharewaka Conference Centre in Wellington, amid some stormy weather. That didn’t deter a large group of ophthalmologists, optometrists and retinal nurses from gathering to discuss the latest research, innovations and challenges in eyecare. Continuing the tradition of previous years, it was more than just a series of talks – it was a deep dive into the evolving landscape of eye health in Australasia and beyond, enriched with clinical pearls that will help shape the future of our practice.
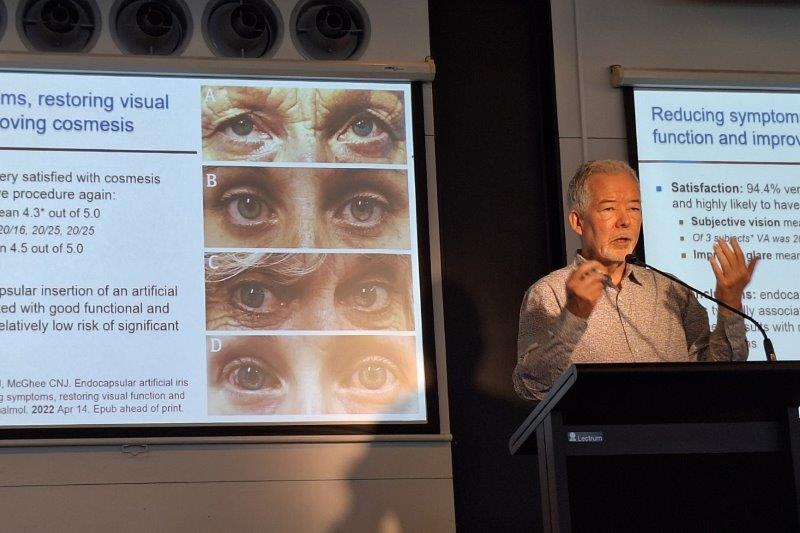
The symposium opened with an insightful presentation by the University of Auckland’s Professor Charles McGhee, who tackled the ever-relevant topic of getting started with research. His words resonated particularly with those of us who balance clinical duties with a desire to contribute to academic knowledge. One striking point he made was the disparity between registrars’ and consultants’ views regarding the necessity of research. While most (93.3%) registrars and fellows surveyed said they feel research is a requirement, only half (46%) of the consultants said they think more training for research is needed, with non-academics showing a stronger belief that research is a requirement.
Prof McGhee explained that research doesn't necessarily begin with a ‘Eureka!’ moment but often with a simple ‘that’s interesting’ thought. This underscored the importance of curiosity in clinical practice. He outlined key considerations for those interested in research, such as finding a suitable mentor, choosing the right topic and the importance of forward planning. His advice on steering clear of poor mentors – which he referred to as “avoid the turkey!” – was a reminder that mentorship can make or break a research journey.
Advancements in glaucoma
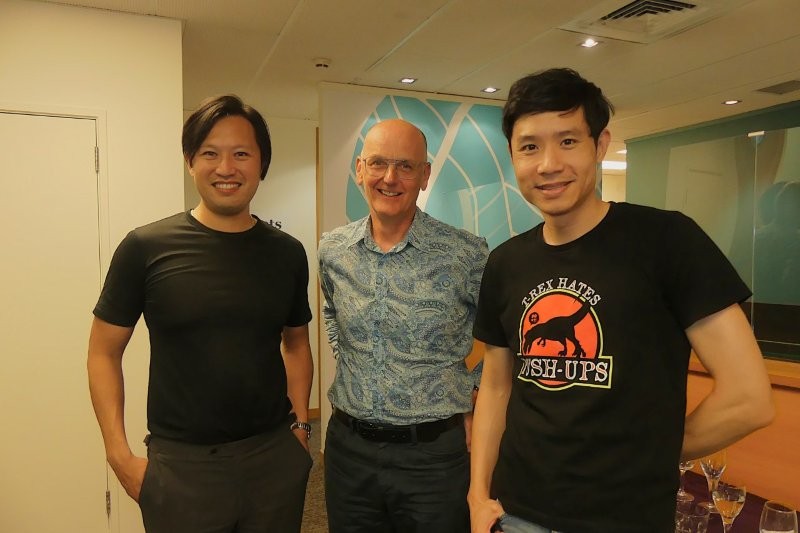
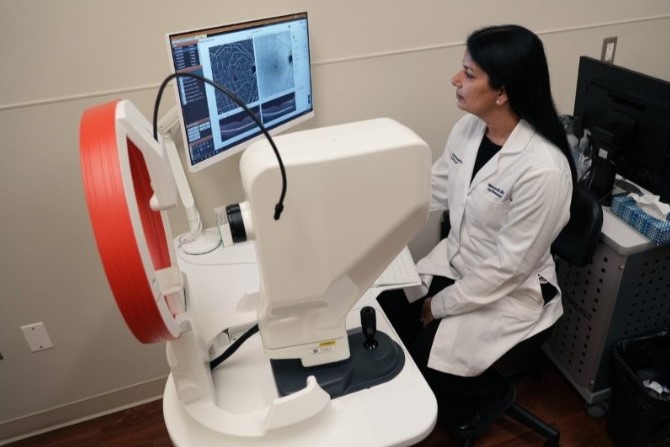
Frequently termed ‘the silent thief of sight’, glaucoma was a major theme this year. Sydney glaucoma and cataract surgeon
provided a fascinating update on the use of optical coherence tomography angiography (OCTA) to examine peripapillary vasculatures. Dr Raniga highlighted the current limitations in our understanding of the relationship between OCTA findings and visual field progression – a gap in knowledge that needs to be bridged before these tools can be fully integrated into routine clinical practice. Her talk reminded those present of the importance of not just adopting new technologies, but also of the necessity for ongoing research to validate their clinical use.

Drs Aparna Raniga, Ainsley Morris and Charisse Kuo
Dr Jesse Gale's presentation on the effects of head position on intraocular pressure (IOP) and intracranial pressure (ICP) added another layer to our understanding of glaucoma management. Dr Gale explored whether patients could benefit from using wedge pillows to modulate these pressures during sleep. The potential to manage glaucoma through such simple, non-invasive means is intriguing, though further investigation is still warranted, Dr Gale pointed out.
The importance of robust data in shaping eyecare policy was highlighted by Dr Cam Loveridge-Easther’s presentation on the Eye Care Situation Analysis Tool (ESCAT) for New Zealand developed between November 2021 and January 2022 by Associate Professor Jacqueline Ramke and her team. Dr Loveridge-Easther’s assessment revealed gaps in our current eyecare system, particularly in health information systems and population surveys on eye conditions. For instance, ESCAT rated the quality and efficiency of eyecare services at a level 2/4.
This was a sobering reminder that, despite the advances we celebrate, there are still significant areas needing improvement, particularly in terms of data collection and reporting. The comparison with the 2023 review of the Australian and New Zealand Neonatal Network (ANZNN), which has made significant strides in data collection and knowledge translation, highlights how much potential there is to improve our own eyecare systems through better data management.
Therapeutic innovations: optimism and caution
The symposium’s updates on therapeutic developments offered reasons for both optimism and caution. In an enlightening and sobering presentation, consultant ophthalmologist at Wellington and Hutt public hospital’s Dr James Leong discussed current and emerging treatment options for geographic atrophy (GA) in age-related macular degeneration (AMD). Intravitreal complement inhibitors such as Syfovre and Izervay have shown promise in slowing anatomical progression, but their benefits come with significant risks, including an increased chance of developing wet AMD.

Dr James Leong
Dr Leong’s critical analysis of the data from phase 2 clinical trials for Annexon Biosciences’ ANX-007 – particularly his comments on the "shrewd" interpretation of results – was a stark reminder of the importance of critical thinking in evaluating new treatments. His conclusion that the current risk-benefit-cost ratios do not favour widespread use of these treatments for most patients –the discontinued development of GT005 by Novartis being a prime example – is a cautionary note for clinicians eager to adopt the latest therapies to improve their patients’ quality of life.
On a more optimistic note, the introduction of Vabysmo (faricimab) as a potential alternative to Eylea (aflibercept) for neovascular AMD was discussed by Dr Leo Sheck. His analysis provided valuable insights into the potential of this bispecific antibody to reduce treatment burdens through less frequent injections. However, the lack of significant visual acuity differences between Vabysmo and Eylea suggests that it may be prudent to continue with the latter until Vabysmo becomes more accessible through Pharmac funding.
Taken together, the presentations by Dr Leong and Dr Sheck emphasised the need for continued research into novel and efficacious treatment for complex ocular diseases such as AMD.
The human side of innovation
Dr Andrea Vincent’s recounting of Ciro’s journey with Leber congenital amaurosis (LCA) was a poignant reminder of the human impact of our work. Gene therapy, still in its infancy, gave this patient the gift of preserving his remaining vision – a rare and remarkable success story in the world of inherited retinal disorders. This story underscored the potential of gene therapy to transform lives, even as we acknowledge the many challenges that lie ahead in making such treatments widely available.
The community-oriented discussions at the symposium, particularly those led by retinal nurse David Garland and Wellington optometrist Ravi Dass, highlighted the importance of accessible eyecare. Garland’s account of the evolution of nurse-led intravitreal injection clinics over the past decade was a testament to how expanding the roles of allied health professionals can increase service capacity. His description of the dramatic increase in intravitreal injections administered by the former Auckland District Health Board – from fewer than 2,000 in 2010 to more than 18,000 in 2023 – powerfully demonstrated the significant impact of these clinics on patient care. Referring to the Friday afternoon injection clinic as "Purgatory", Garland humorously captured the relentless pace of the environment.
Dass’ work with the Foureyes Foundation, which seeks to remove barriers to eyecare for children, was particularly inspiring. By partnering with iwi-led medical centres and local schools, the foundation has made significant strides in providing vision screenings, eye tests and glasses to children who might otherwise slip through the cracks. His approach, which involves leaving autorefractors in schools for easier data sharing and prioritising children in low-cost clinics, offers a model for more accessible and equitable eyecare.
A call to address inequities
Dr Micah Rapata’s qualitative kaupapa Māori review of the Auckland Crosslinking Service to identify barriers and enablers for Māori patients with keratoconus was both confronting and timely. Dr Rapata’s study identified several key challenges, including travel costs, inconvenient appointment times and language barriers, highlighting the need for culturally responsive care and improved accessibility for Māori patients.
One of the most thought-provoking talks of the symposium came from oculoplastic and orbital surgeon Dr Stephen Ng, who challenged us to reflect on "institutionalised behaviours" in our practice. His candid discussion about the ingrained biases that can lead to inequities in care, such as the belief that half of his Māori patients would not show up for appointments, was a wake-up call. Dr Ng’s assertion that such behaviours can become so normalised that we stop questioning them was a powerful reminder of the need for ongoing self-reflection.
Dr Ng’s call to action, “If we can recognise it, we can fight barriers and change the society”, was a fitting conclusion to the symposium. His message that “If everyone just changes one thing…” encapsulated the ethos of the Save Sight Symposium: continuous improvement, both in our clinical practice and in how we engage with the broader community.

Janice Yeoman and Dr Stephen Ng
Looking ahead
This year’s Save Sight Symposium was a rich tapestry of ideas, innovations and reflections. From cutting-edge research in glaucoma and AMD to community initiatives that make eyecare more accessible, it provided a comprehensive overview of where we stand and where we need to go. It was a great reminder of the importance of curiosity, critical thinking and community engagement in our work. The future of eye health will be shaped by the research we pursue, the therapies we develop and the care we provide to our patients. It is up to each of us to ensure that we are moving in the right direction.

Dr Lola Mugisho is a senior research fellow and deputy director of the Buchanan Ocular Therapeutics Unit at Auckland university. Her research involves developing pre-clinical models to test the efficacy of novel anti-inflammatory therapeutics for the treatment of age-related neurodegenerative diseases affecting the eye and brain.

Dr Charisse Kuo is a therapeutically qualified optometrist in the final year of her PhD at the University of Auckland. Her research involves the development of tissue-culture models using donor retinas and choroids to explore the mechanisms behind diabetic retinopathy.