OTC 2023: drops, shots and supplements
It was exciting to see fellow optometrists and ophthalmologists catching up with each other at this year’s Ocular Therapeutics Conference at the University of Auckland given the long, quiet period due to the pandemic. Despite the chaos brought by Cyclone Gabrielle, there was a great turnout, so it was good to see so many familiar faces in the same space once again.
Covid complications and cataract risks
The first session took us back to the pandemic and how Covid-19 can impact the eye. It was reassuring to learn the receptor to which Covid spike proteins attach (angiotensin-converting enzyme-2 ACE2) has greater expression in the posterior eye and is absent on the ocular surface, which means it’s unlikely the virus can directly infect the ocular surface. However, Dr Michael Wang said it is possible for the viral particles to enter the eye via the nasopharyngeal sinus, connected to the nasolacrimal sinus. It was also somewhat frightening to learn about ocular complications which can be incited by Covid vaccination, including virtually any inflammatory eye disease, such as uveitis, toxoplasmosis and even central retinal vein occlusion. The key take-home messages included:
- Consider Covid vaccination as a possible cause of inflammatory eye disease or retinal vascular occlusion
- Diagnose by exclusion – investigate other causes first and never make assumptions
- Counsel and take note of patients who have poorly controlled Covid symptoms and a history of ocular side-effects post-vaccination
- Vaccination is still usually preferable to Covid infection
The second session focused on the lens. It was reassuring to know Auckland’s ophthalmologists regularly audit using the New Zealand Cataract Risk Stratification system, which significantly reduces the overall risk of cataract surgery complications. Dr Mo Ziaei shared videos of surgeries complicated by dense cataract, capsular tears, endothelial trauma and corneal oedema, talking us through the additional steps he would add for these specific high-risk groups and the amazing outcomes that can be achieved. He stressed the importance of educating such patients and setting expectations, especially regarding post-operative events such as raised intraocular pressure (IOP), rebound or persistent post-op inflammation, cystoid macular oedema, pseudophakic bullous keratopathy and endophthalmitis.
Antioxidants, Vuity and dealing with certain eye diseases
On the flip side, Dr Julie Lim presented her research on nutrient and antioxidant delivery to the centre of the lens. She showed us that cysteine, a component of glutathione (the primary antioxidant in the lens), can itself act as an antioxidant. Thus, targeting the cysteine transporter may be a therapeutic route for enhancing antioxidant delivery, potentially slowing cataract formation.
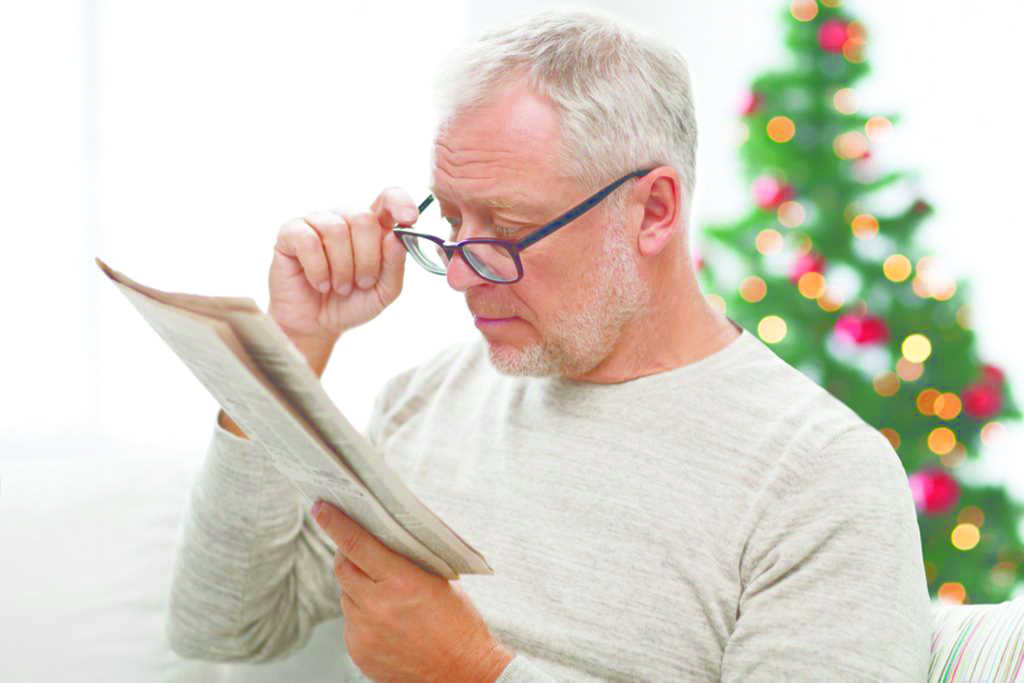
Dr Trevor Gray introduced us to Vuity, the first US Food and Drug Administration-approved eye drop to reduce presbyopic symptoms. Containing 25% pilocarpine, Vuity’s mechanism is based on the miosis-induced pinhole effect, which increases depth of focus. Dr Gray said this will be a game changer, attracting patients who had never walked into an optometrist clinic prior to being struck by presbyopic symptoms. However, as optometrists, we need to be aware of side effects and contraindications such as myopic shift, brow-ache, dimming due to miosis and retinal detachment, he said.
The third session focused on the chronicity of external eye diseases. Dr Bia Kim educated us on the careful treatment and management of patients with ocular cicatricial pemphigoid, graft versus host disease and Stevens-Johnson syndrome – autoimmune diseases that are poorly understood. Next, Dr Graham Reeves reminded us of the importance of minimising glaucoma’s impact on patients’ lives by avoiding significant vision loss and making sure treatments do not affect the quality of life through direct side effects or psychological burden (see more on this on p18).
Dr Simon Dean then talked about off-label use of Zematop 0.1% (tacrolimus) for vernal keratoconjunctivitis. This steroid-sparing agent indicated for atopic dermatitis is now available in New Zealand for $5 on special authority prescription. However, it is well known that ocular steroid use can cause IOP issues and skin thinning, both undesirable risks for vernal patients who are usually young children requiring chronic treatment. Dr Dean warned the ointment stings for the first two weeks but if successful can replace all topical treatment with once-daily dosage in vernal patients. Dr Hussain Patel closed the session by sharing the complicated case of a glaucoma patient with atopic keratoconjunctivitis, which required steroid treatment, leading to IOP rise and necessitating a change of glaucoma drops.
Zinc to new depths
My favourite talk of the conference was Dr Rachel Barnes’ 'Supplements for age-related macular degeneration (AMD) – are they useful?’ This has always been a topic of debate and I often question whether there are benefits to such supplements. Dr Barnes presented us with results from the age-related eye disease study (AREDS) and AREDS2, with the main take-homes being:
- Beta-carotene (a vitamin A precursor) with 80mg zinc reduced the risk of advanced AMD by 25% but worsens lung cancers in smokers
- Lutein and zeaxanthin are beneficial, especially if you don’t concurrently give beta-carotene (due to competitive absorption)
- 80mg or 25mg zinc seem to deliver the same effect, although 25mg is more tolerable for most patients
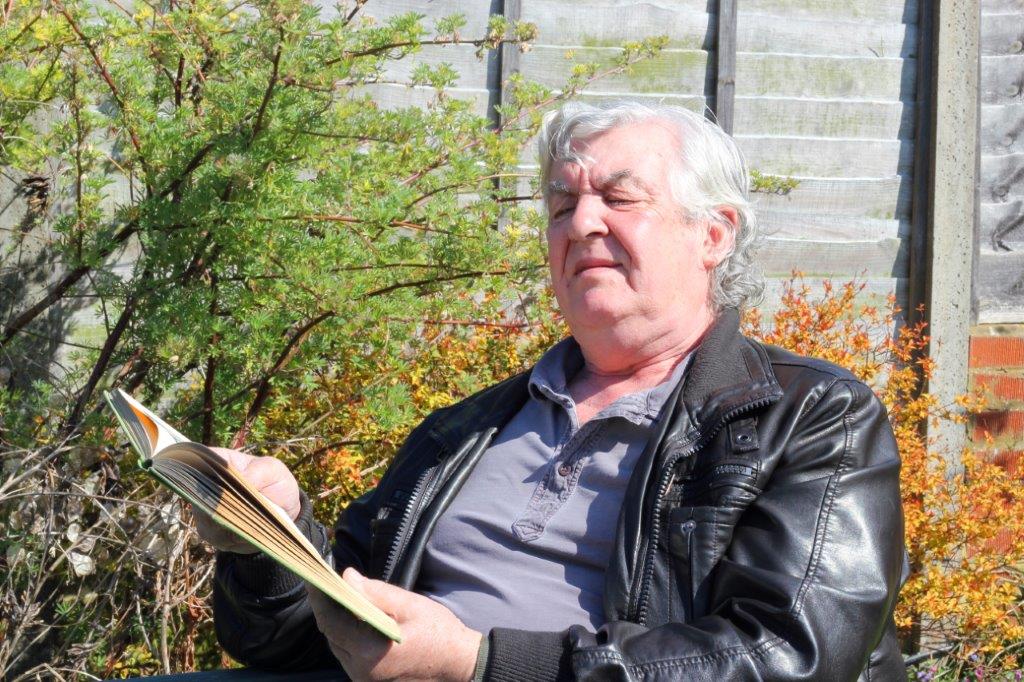
Dr Barnes recommended that everyone eats a good diet, “just like your mum told you”, and explained this in the context of a healthy gut microbiome maintained by micronutrients from food. “Everybody benefits from a good diet, everybody benefits from not smoking,” she said. Additionally, she said she would recommend supplements for at-risk patients who want to be doing everything they possibly can, making it clear that while they will not have a big effect and are not guaranteed to work, they may be beneficial in reducing the risk of developing severe AMD.
Dry eyes to herbal enemies
Professor Jennifer Craig talked about different natural therapeutic options for dry-eye disease (DED), explaining that there is far too much omega-6 in our diet but ingesting more omega-3 can help prevent omega-6 breaking down into pro-inflammatory metabolites. She advised making sure patients are not going overboard, however, since too much omega-3 can affect blood clotting. Associate Professor Ilva Rupenthal then discussed a range of preservative-free artificial tears, the differences between them and the mechanisms by which some preserve the lipid layer or the tear film.
Wrapping up, Dr Rasha Altaie shared a story about the inappropriate use of natural remedies which she encountered on the first day of her fellowship with Professor Charles McGhee in 2008. A 36-year-old woman had presented with a melted cornea and severe stem cell deficiency after applying crushed ‘lacropoly’ 1gt on each eye daily for a week. Lacropoly was revealed to be jasmine (lady of the night), commonly found in New Zealand gardens. Laboratory results showed it contained 17 types of steroid and a high concentration of alkaloid, which was most likely what killed her corneal stem cells. New Zealand does not have specific legislation to regulate complementary and alternative medicine practitioners, warned Dr Altaie, which includes those practicing acupuncture, aromatherapy and chiropractic. While there is definitely room for these, we first need to collect data to know what is safe, what works and what doesn’t, she said. This triggered some heated discussion, especially given some New Zealand midwives still advise new mums to put breastmilk into their babies’ eyes because it is ‘healthy’. Clearly improvement is required, even in regulated health professions!
Charisse Kuo is a therapeutically qualified optometrist in the final year of her PhD at the University of Auckland. Her research involves the development of tissue-culture models using donor retinas and choroids to explore the mechanisms behind diabetic retinopathy.