Illuminating Nightingales – The RANZCO AONA conference
As it was the first face-to-face RANZCO Congress in three years, the Queensland Branch of the Australian Ophthalmic Nurses Association (AONA) organised a sister conference including wide-ranging topics and opportunities for some overdue catching up. Having registered for both the nurses’ and the main RANZCO conference, I was able to attend several sessions, including the Dame Ida Mann Memorial Lecture by Professor Helen Danesh-Meyer, who presented research with the potential to change the diagnosis, treatment and outcomes for not only ophthalmology patients, but also neurological patients.

Prof Helen Danesh-Meyer accepting the Dame Ida Mann Memorial Lecture Award from Prof Charles McGhee
It was great to see former Aucklanders in attendance, including Drs Shuan Dai and Jennifer Fan Gaskin, plus a nurse from Auckland City Hospital now doing ophthalmology. Having time to go around the trade exhibitions allowed me to visit the Northern Territory Mobile Eye Unit, which provides services to rural and remote Australia. The unit offers three distinct areas – examination, investigation and laser.
The nurses’ programme had a total of nine presentations, of which three were from nurses. The most relevant and potentially concerning presentation for ophthalmic nursing came from Dr Heather Machin from Melbourne’s Centre for Eye Research Australia (CERA). She undertook a national survey, sponsored by AONA, which found 69% of nurses working in the eye arena intend to retire in the next 10 years, which is likely to be reflected in New Zealand.
Cataract action
Dr James Pietrie delivered another topical presentation, having undertaken research into the surgical waste generated in cataract surgery. Although some other surgical specialties generate more waste per procedure, the number of cataract procedures undertaken means it warrants scrutiny. Dr Pietrie highlighted other considerations, namely the ways different countries’ standards of practice impact surgical waste and the ability to make significant change. Interestingly, the research appeared to overlook the environmental impact of agents used to clean and sterilise items if they were reused or had a low fiscal impact.
Dr Stephen Godfrey gave a very enthusiastic presentation on the complications of cataract surgery. He spent the first 10 minutes stressing the importance of pre-operative preparation for a successful outcome. He recommended patients with dry eyes be sent home with lubrication drops for one month before re-doing biometry to ensure best possible measurements are available. Equally important was the pre-op discussion around the patient’s visual outcome expectation. “We have all had the patient that sits in the vision lane and is disappointed that their vision is not perfect for both distance and reading vision,” said Dr Godfrey. Of his many pearls of wisdom from years of cataract surgery, managing patient expectations was paramount.
Surprising Lee patient
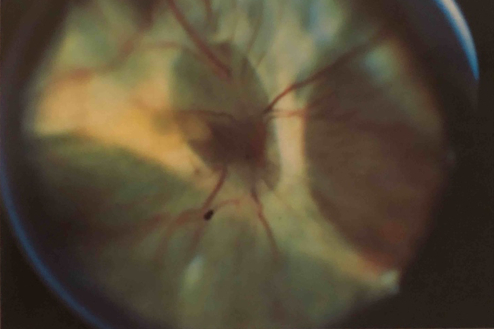
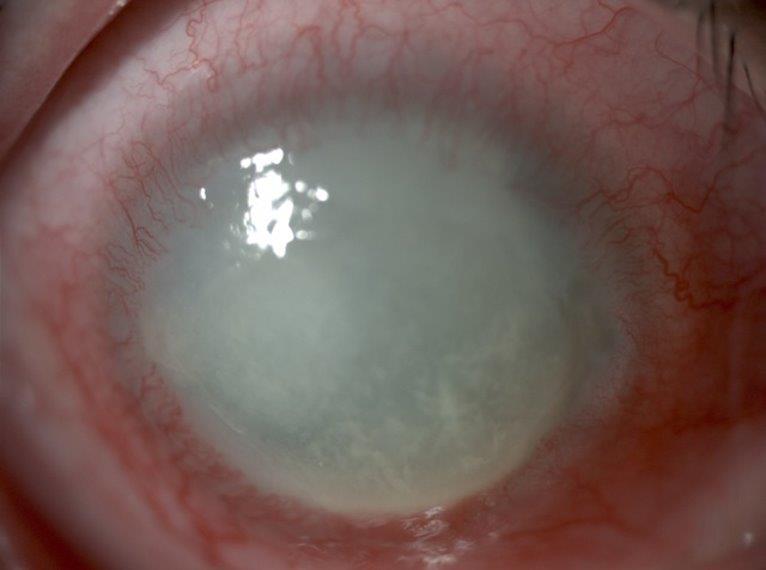
Professor of ophthalmology at The University of Queensland and glaucoma specialist Dr Graham Lee gave a very entertaining presentation titled ‘A Surprise Case’. Although the discussion and video clips of glaucoma patients using and instilling their drops was lighthearted, it came with a very important message about ensuring patients understand compliance and can instil their drops.
The surprise case was a patient who had undergone filtration surgery but subsequent fluid leakage into the orbit caused a very large proptosis when the speculum was removed. An audible gasp was heard in the room when the picture came up on the screen. Neither Dr Lee nor the colleagues he called for advice had seen anything like it. For the first time that Dr Lee could recall, the anaesthetist got out of his chair to check out this unusual occurrence! Following gentle massage of the globe and surrounding tissue, the proptosis reduced within 30-45 minutes and the lids were able to close to protect the globe, resulting in a good outcome for the patient.
The final presentation I found interesting was Brisbane retina surgeon Dr Tom Moloney’s ‘An update on the world of retina’. He discussed promising potential treatments for age-related macular degeneration, with alternatives to injection or agents that extend the time between injections, which everyone is hoping are on the horizon.
Sue Raynel is a part-time staff nurse in the Eye Clinic at Greenlane Clinical Centre, with more than 30 years’ experience in ophthalmology. She presented ‘Nightengalism into the Future’ at the AONA conference, reflecting on technological changes to practice over the last 30-40 years, changes in hospital stays for cataract surgery from 5-7 days to hours, and the introduction of advanced practice roles.