Corneal donation and corneal transplantation in Aotearoa
Despite attempts since the early 1800s, success in corneal transplantation remained elusive until the
beginning of the 20th century. Indeed, corneal transplantation is the oldest form of tissue transplantation with the first successful full-thickness corneal transplant performed by Eduard Zirm in 19051. Zirm’s perspicacity paved the way for the success of contemporary corneal transplantation, which is primarily the result of a culmination of pivotal achievements, including the introduction of corticosteroids in the 1950s, the refinement of suture materials in the 1960s and the development and wider employment of surgical microscopes in the early 1970s1.
Indications for corneal transplants
The three most common indications for corneal transplantation in New Zealand in 2019 were repeat transplant (30.9%), keratoconus (27.9%), and corneal dystrophies (18.8%), of which the majority were Fuchs’ endothelial corneal dystrophy (92.8%) (Figs 1 and 2)2. Bullous keratopathy as an indication sits at a historic low of 7%, likely due to improved cataract surgery techniques over the last three decades. Regrafts surpassed keratoconus for the first time in 2019, which was previously the leading indication for keratoplasty since New Zealand records commenced, this is secondary to an ageing population who have long-term (exhausted/rejected) corneal grafts (Fig 3), coupled with an increased failure rate following the initial introduction of newer lamellar techniques2.
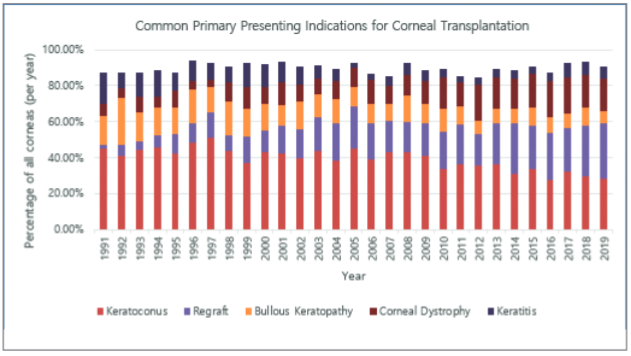
Fig 1. Common primary presenting indications for corneal transplantation as a percentage of all corneas transplanted annually in New Zealand
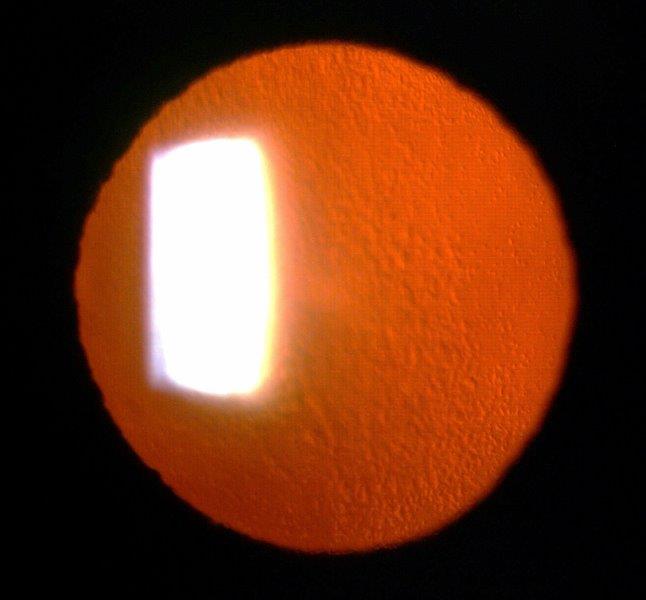
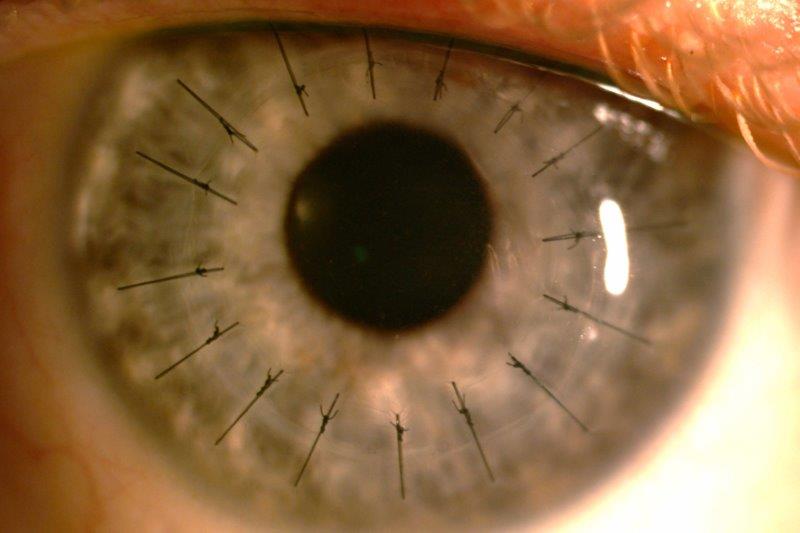
Fig 2. Retro-illumination of a cornea showing multiple guttata in a case of moderate Fuchs Endothelial Corneal Dystrophy –
now one of the most common indications for corneal transplant in NZ
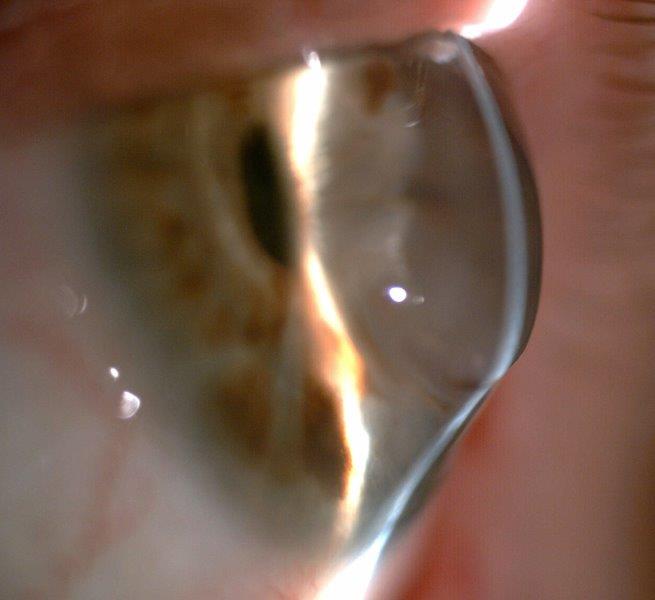
Fig 3. A failing, 30-year-old penetrating keratoplasty for keratoconus with extreme inferior ectasia
Corneal transplant techniques
The total number of corneal transplants performed annually in New Zealand from 1991-2020 has steadily increased, with a significant increase in the utility of lamellar corneal surgery (approximately 50%) over the last two decades, including: deep anterior lamellar keratoplasty (DALK), Descemet membrane endothelial keratoplasty (DMEK) and Descemet stripping (automated) endothelial keratoplasty (DS(A)EK)2. This is largely due to the growing number of indications amenable to treatment by lamellar keratoplasty and adoption of newer transplantation techniques to replace only anterior or posterior corneal layers.
Establishing the New Zealand National Eye Bank
In Aotearoa, the first human corneal transplant was successfully performed by Dr Cecil Pittar in 1949, and the procedure was subsequently more widely popularised in the early 1970s3. Notably, the New Zealand National Eye Bank (NZNEB) was founded by Dr Gillian Clover in 1989, with Dr David Pendergrast as its clinical director3. The NZNEB is a charitable, non-profit organisation dedicated to the prevention of blindness through the acquisition, storage and distribution of donated corneal and other tissues throughout New Zealand. All NZNEB operations comply with the standards of the Eye Bank Association of Australia and New Zealand (EBAANZ)4.
The NZNEB ensures that donor corneas are distributed in an equitable manner and it has provided the vast majority of donor tissue for corneal transplantation in Aotearoa over the last quarter of a century. Transplantation numbers have increased dramatically from approximately 240 (2002) to 300 (2019) per annum pre-Covid5. It is now anticipated that at least 350 transplants per year are required, despite a very significant downturn in all forms of tissue donation, beginning a decade ago. The NZNEB also maintains a prospective database that is crucial for monitoring donated corneal tissues in New Zealand and this has led to many scientific publications in the international literature.
Donation process
Therapeutic human tissue transplantation is governed by the Human Tissue Act 2008, where consent is paramount to any form of collection or use of human tissue. Donation by family or whānau is entirely voluntary and the final decision pertaining to donor status and tissue use is made by the next of kin, irrespective of donor wishes or status on their driver’s licence.
During the referral process, NZNEB usually receives a notification from Organ Donation NZ that an individual has died and has met preliminary criteria for donation. If the individual was a consenting donor, in most cases the eye bank can arrange for retrieval immediately. Otherwise, the eye bank contacts the next of kin to obtain consent. In either case, the NZNEB will contact the next of kin to obtain a medical history to determine donor eligibility, as well as obtaining relevant medical records from the hospital. Corneal retrieval is typically arranged as soon as practical after death or within 24 hours.
Criteria for corneal donation in New Zealand
As part of the EBAANZ, the NZNEB adheres to a common set of medical standards regarding the assessment of donor suitability and applies certain exclusion criteria6. Unlike in organ donation, age and blood type are unimportant in determining cornea donor suitability. Similarly, donor eye colour and eyesight quality are not barriers to donation6. With the exceptions of a few pre-existing conditions, such as HIV and infective hepatitis, most causes of death do not impact the ability to donate. Corneal tissues are generally much more resistant to the effects of hypoxia than solid organs, which allows time for a more comprehensive risk assessment, including a medical history review, serological testing and evaluation of endothelial viability6.
Contraindications for tissue donation include but are not limited to: death from an unknown cause; infectious diseases such as HIV, hepatitis B and C; various neurological disorders, such as dementia and multiple sclerosis; systemic viral infections; leukaemia; lymphoma; and prior corneal surgery6.
Sources of corneal donation in New Zealand
As seen in Fig 4, there has been a dramatic decline in the amount of tissue donation from the Coronial Service since 2005, with it accounting for less than 5% of the total number of donor tissues since 2016. While public hospitals have subsequently been the predominant source of tissue donation in New Zealand in the last 15 years, unfortunately, there has been a worrying, gradual decline in corneal donation numbers since 2017. Consequently, the number of donor tissues imported from overseas to counter this decline has increased markedly in the last four years, with Australian Eye Bank sources now accounting for almost 50% of all donor tissues supplied in Aotearoa in 2021, at considerable additional cost.
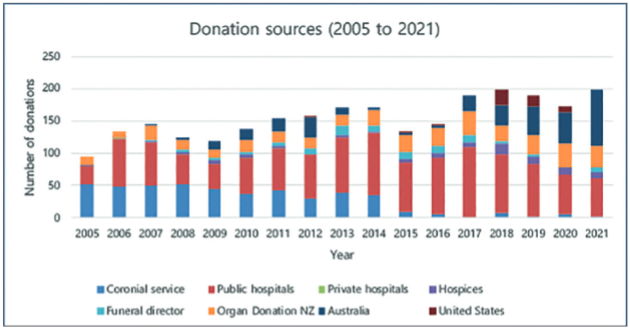
Fig 4. Corneal tissue donation sources in NZ from 2005 to 2021. Credit: The NZNEB
Number of corneal donors and corneal transplantation
The US has the highest rate of corneal donation globally at 366 per million, while the UK has a rate of 100 per million7. In comparison, New Zealand and Australia have significantly lower donor rates at approximately 80 per million, though still higher than the median rate of 55 per million in participating Organisation for Economic Co-operation and Development (OECD) countries7. In terms of the distribution of corneal transplantations, New Zealand performs 63.0 corneal transplantations per million population per year, which is comparable to Australia (65.8), and the UK (61.3) but slightly lower than Singapore (77.7)7.
Other services provided by the NZNEB
The NZNEB also supplies sclera to be used with orbital implants after enucleation, emergency patches for perforated eyes, and for glaucoma surgery. Amniotic membranes are used as transplants, biological bandages and cell carriers for limbal stem cell deficiency8.
With additional consent from the next of kin, and without impacting tissue supply for corneal transplantation, the NZNEB also supports research to better understand eye diseases and to achieve better treatments. Tissues used for this purpose include those not suitable for transplant and residual tissue post-transplantation. Current research projects include the investigation of alternative sources of corneal endothelial cells with peripheral rims of donor corneal tissue post transplantation, the inflammatory pathway of diabetic retinopathy using donor retina and lens physiology using donor crystalline lenses. In recent years, a novel algorithm for corneal endothelial viability analysis has been developed by the Eye Bank’s technical officer, Nigel Brookes, which facilitates reliable and rapid measurement of corneal endothelial size (polymegathism) and shape (pleomorphism)9.
Current issues in provision of corneal tissue
There has been a dramatic increase in the number of corneal transplants in the last three decades as a result of substantial population growth, the burgeoning numbers of cataract procedures in an increasingly elderly population, the prevalence of keratoconus and widespread adoption of endothelial keratoplasty at earlier stages of endothelial corneal diseases (Figs 5 and 6)2. Conversely, there has been some easing in demand with the introduction of corneal crosslinking for keratoconus, and an improvement in cataract surgery techniques with decreased incidence of bullous keratopathy2.
Unlike our counterparts in Australia, who actively screen all deaths as potential eye donors via their DonateLife network, there is a lack of similar donor screening programmes here. The diminishing numbers of donors sourced from the Auckland Coronial Service continue the trend observed in previous decades, and is secondary to reducing numbers of post-mortems in New Zealand4. In response to this trend, donor programmes were established at public hospitals and there was an increase in donors sourced via Organ Donation NZ, which is a subsidiary of the NZ Blood Service. Historically, corneal donation rates in New Zealand have been low and the challenge is further compounded by the Covid-19 pandemic in the last two years. Due to the pandemic, Australian Eye Banks are also currently facing their own struggles to fulfil their domestic corneal transplant requirements and consequently, despite the exceptional support of NZNEB, from time to time they are unable to supply any donor tissue to New Zealand. Thus, the waiting time for corneal transplantation has increased substantially over the last two years.
The NZNEB operates a 24-hour, 365-day service to coordinate eye donations from hospitals and the community around the country, therefore operating costs are high. However, it only receives government funding for approximately 25% of operating costs. As such, with vastly increased costs in the retrieval, processing, storage and provision of tissue in recent years, maintaining fiscal security of NZNEB is a continuing challenge.

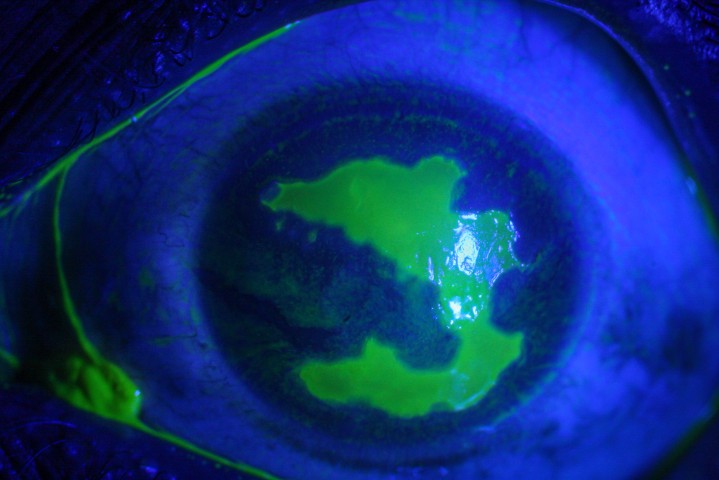
Fig 5. Slit lamp view of an ultrathin DSAEK at three months in Fuchs’ endothelial corneal dystrophy
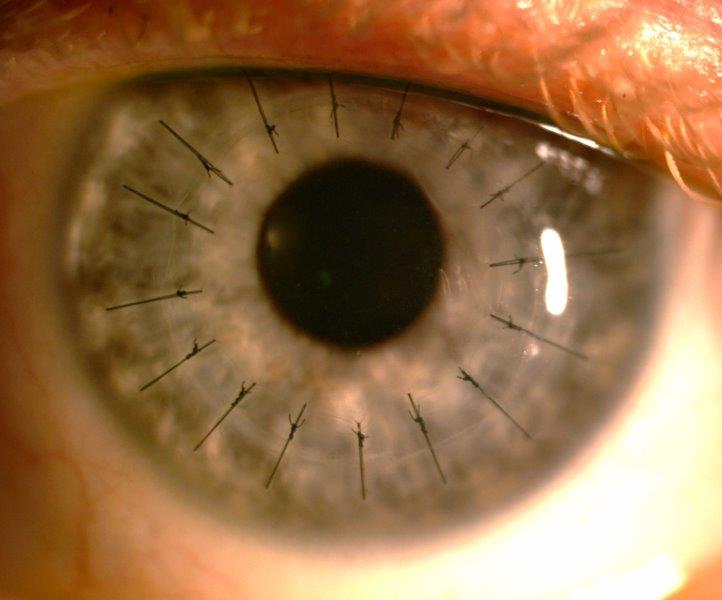
Fig 6. A penetrating keratoplasty one month after surgery for previous microbial keratitis with associated,
extensive para-central corneal scarring
Proposed solutions
At present, Organ Donation NZ’s primary focus is on solid organ transplantation via intensive care units (ICUs), and there is a crucial lack of tissue-specific donor programmes in New Zealand. Efforts are being made to set up a system which will allow active screening of all deaths as potential eye donors outside of ICUs as well as hospices, especially in Auckland. Additionally, there should be considerable effort to cultivate and strengthen relationships with donation sources while creating a two-year plan to be self-sufficient. In the aftermath of the pandemic, understanding public attitudes pertaining to corneal donation and creating awareness of the substantial benefits of corneal donation is also important.
Who runs the NZNEB?
Maria Fung joined the NZNEB in March 2022 as the business manager when Louise Moffatt stepped down after 20 years of service. Key staff include Nigel Brookes and donor coordinators Helen Twohill and Maureen Watson. An additional coordinator or clinical manager is currently being recruited. The NZNEB has five trustees which include Prof Charles McGhee (scientific director and chair), Dr David Pendergrast (clinical director), Dr Andrew Logan (Wellington), Dr Logan Mitchell (Dunedin) and Dr Peter Ring (Auckland).
Conclusions
Corneal transplantation has long been established as the most common, and indeed the most successful, form of human transplantation. A multitude of factors have translated to a significant increase in the demand for donor tissue in New Zealand in the last 30 years. Subsequently, the NZNEB faces an uphill battle to meet this demand, given New Zealand’s low cornea donation rate and the advent of Covid-19. Obtaining donor tissue from overseas to address the substantial shortage is, and should only be, a temporary measure. To achieve self-sufficiency, it is paramount to implement New Zealand donor screening programmes, and develop an integrated approach among local donor services, medical professionals and the community.
References
- Crawford AZ, Patel DV, McGhee CN. A brief history of corneal transplantation: From ancient to modern. Oman Journal of Ophthalmology. 2013 Sep;6(Suppl 1):S12.
- Chilibeck CM, Brookes NH, Gokul A, Kim BZ, Twohill HC, Moffatt SL, Pendergrast DG, McGhee CN. Changing trends in corneal transplantation in Aotearoa/New Zealand, 1991 to 2020: Effects of population growth, cataract surgery, endothelial keratoplasty, and corneal cross-linking for keratoconus. Cornea. 2021 Jul 15.
- Hadden B. Eye surgeons and surgery in New Zealand. Penguin Random House New Zealand Limited; 2014 Nov 7.
- Cunningham WJ, Moffatt SL, Brookes NH, Twohill HC, Pendergrast DG, Stewart JM, McGhee CN. The New Zealand National Eye Bank study: trends in the acquisition and storage of corneal tissue over the decade 2000 to 2009. Cornea. 2012 May 1;31(5):538-45.
- Patel HY, Ormonde S, Brookes NH, Moffatt SL, Sherwin T, Pendergrast DG, McGhee CN. The New Zealand National Eye Bank: survival and visual outcome one year after penetrating keratoplasty. Cornea. 2011 Jul 1;30(7):760-4.
- Eye Bank Association of Australia and New Zealand. Guidelines for the medical selection of ocular tissue donors. Aug 2019 [cited 2022 Mar 2]. Available from: https://ebaanz.org/wp-content/uploads/2021/05/EBAANZ-Donor-Selection-Guidelines-2019.pdf
- Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, Thuret G. Global survey of corneal transplantation and eye banking. JAMA ophthalmology. 2016 Feb 1;134(2):167-73.
- Harkin DG, Apel AJ, Di Girolamo N, Watson S, Brown K, Daniell MD, McGhee JJ, McGhee CN. Current status and future prospects for cultured limbal tissue transplants in Australia and New Zealand. Clinical & Experimental Ophthalmology. 2013 Apr;41(3):272-81.
- Brookes NH. Morphometry of organ cultured corneal endothelium using Voronoi segmentation. Cell and Tissue Banking. 2017 Jun;18(2):167-83.

Dr Aaron Ong is the Maurice and Phyllis Paykel corneal and anterior segment clinical research fellow in the Department of Ophthalmology, University of Auckland (UoA).

Dr Jie Zhang is a senior HRC research fellow and scientist in the Dept. of Ophthalmology, UoA. She has specific research interests in both laboratory and clinical aspects of the cornea and anterior segment.

Nigel Brookes is a senior technical officer at the NZ National Eye Bank.