Getting to grips with allied health priorities
New Zealand’s first chief allied health professions officer Dr Martin Chadwick was appointed in February 2019. His challenges include improving health equity and transdisciplinary working, both hot topics within the eyecare community. Drew Jones found out how it’s all going.
Will scope changes help reduce Aotearoa’s backlog of cataract and diabetic retinopathy patients?
The number of patients waiting for planned care interventions like cataract procedures has been an area where the health system needs to change service delivery to reduce the backlog. I can see the full scope of optometrists’ skills being used in eyecare pathways, including the extension of their clinical scope to enable improved prescribing, and utilising them to support the provision of intravitreal injections for macular degeneration.
Improving collaboration and integrated models of care between general practice, ophthalmologists and optometrists is another way to improve planned care for patients. For example, collaborative referral guidance between the professions and increased use of telehealth for brief optometry consults.
You’ve said digital literacy should be part of health training programmes – how will that manifest in orthoptics and optometry?
The current state of digital integration within optometry and consumer involvement in their care and user-focused services is expanding, (such as) consumer use of online glasses choice. The Hira (National Health Information Platform) development programme intends to provide the ability for private and public providers to contribute their (patients’) data and health information and view it in a single place, in a timely manner.

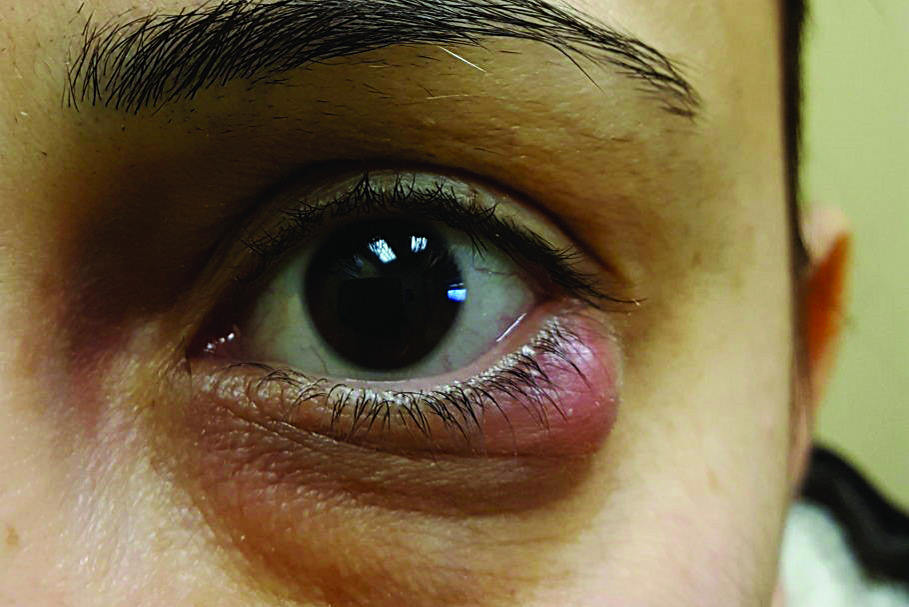
Dr Martin Chadwick, NZ's first chief allied health professions officer
As Health NZ supplants district health boards (DHBs), will that mean more community care?
As we move towards the Māori Health Authority and Health NZ, I believe optometrists will be provided more opportunities, with the change in DHBs moving from a funded-for-services model to the Health NZ model of commissioning for service. A funded-for-services model provides clarity for what you're funding and commissioning provides a requirement to fund for outcomes and, collectively, unmet community needs.
From an optometry perspective, it's about knowing what that potential unmet need in our communities is, such as macular degeneration and cataracts, and looking at how care can be shifted out of a hospital setting and into the community as part of the locality design.
With the proven success of optometrists performing YAG laser, corneal cross-linking and anti-VEGF injection treatments within ophthalmologist-led teams overseas, is there government support for similar upskilling here?
International best-practice and working to the top of their scope of practice is something I strongly encourage and support. This is a great example where I would encourage and support optometrists and ophthalmologists to work together and show joint leadership to improve patient outcomes and access timely care.
Have you been aware of resistance to this from some parts of the eyecare community, especially in Australia?
The argument is not about professional conflict and not about arguing over whose patch it is, but about jointly addressing a population health issue in New Zealand.
I have a close collegial relationship with the other chief clinical officers at the ministry and we are very willing to continue to work collectively across optometry, ophthalmology and nursing. This will involve working through the issues together and ensuring there will not be barriers.
How do we encourage more youngsters from all backgrounds into optometry?
In New Zealand there are disparities in eye health outcomes between Māori and Pacific peoples and other ethnic groups; having a health workforce that reflects the population it serves is critical. But creating an environment in which Māori and Pasifika can thrive is just as important as encouraging people to join the profession.
For any young New Zealander, being able to see a career and work environment where they are contributing to their communities, are provided opportunities and are culturally safe, is important.
What are your goals in 2022?
My role provides a link into the ministry to ensure there is voice for the allied health (workforce). Among our ongoing Covid-19 response and health reforms, my main goal is to continue to see these challenges as an opportunity for allied health to improve health outcomes for priority populations in the community. That means staying true to the priorities on the Allied Health Business Plan, which offers real solutions to how services can be provided more effectively and efficiently, allowing greater (more equitable) access.
The challenge lies in changing the system to be the enabler. If we have learnt nothing else from the Covid-19 period, it is that we can be nimble and can change rapidly when there is a collective will to do so.